Early detection saves lives. Yet, for too many Black women, that opportunity comes too late. Although Black and white women develop breast cancer at roughly the same overall rate, Black women are about 38–40% more likely to die from the disease. That stark difference reflects not biology alone, but deep systemic inequities that affect nearly every step of Black care continuum—from screening and diagnosis to treatment and follow-up.
Research shows that Black women are often diagnosed at younger ages, at more advanced stages, and with more aggressive subtypes, which tends to grow and spread faster and has fewer treatment options. Other factors compound the problem: limited access to high-quality mammography centers, longer wait times for follow-up imaging or biopsy, under-insurance, and medical bias that can delay or downplay symptoms. In some cases, mammograms are interpreted without the benefit of newer technologies—like digital breast tomosynthesis (3D mammography) or even AI-assisted reading—that can better detect cancers in dense breast tissue, which is more common among younger women and Black women.
Too often, Black women’s pain or concerns are dismissed, or they are not informed of the latest screening tools and risk-assessment options. That’s why this new generation of FDA-approved artificial intelligence (AI) technologies represents both a scientific breakthrough and a chance for health empowerment—if we know to ask for it.
Being informed means we can make decisions earlier, push for equitable access to advanced screening, and ensure that bias does not silence or sideline us.
Become Your Own Advocate
We must learn to be our own advocates even before we enter the exam room. Importantly, if you don’t understand the answers, please ask your provider to repeat and speak outside of the medical terminology. If you have a breast cancer screening scheduled, ask your healthcare provider questions such as:
- What kind of mammogram am I getting—2D or 3D?
- Does your facility use AI-assisted reading?
- Am I considered high-risk, and what does that mean for how often I should be screened?
- Do I have dense breast tissue, and if so, how does that affect my risk or the accuracy of my mammogram?
- What happens if my mammograph shoes an abnormality? How quickly will I get the results and a follow-up plan?
- Are there lifestyle changes, medications, or genetic tests that could reduce or clarify my risk?
Being an advocate for yourself also means researching where these advanced technologies are available, requesting copies of imaging reports, and connecting with breast-health organizations that center our voices, such as Sisters Network Inc. and Black Women’s Health Imperative. Educating yourself and becoming a part of targeted communities means not waiting for the system to catch up, but demanding the same level of precision, attention, and innovation that others already receive.
The emergence of AI-powered imaging and risk-prediction tools marks a new frontier in breast cancer detection. But to truly save lives in our communities, technology must be a part of self-advocacy—and both must be rooted in awareness, access, and action.
AI-Driven Screening Tools Cleared by FDA
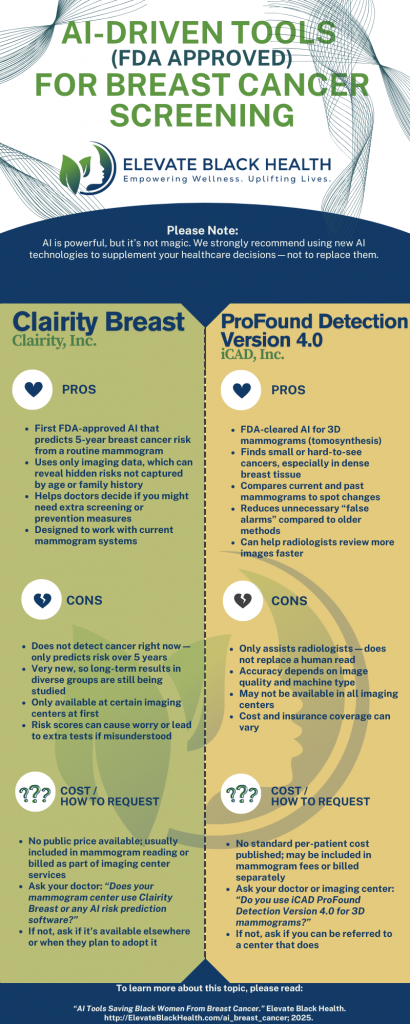
Over the past year the U.S. Food and Drug Administration (FDA) has stepped up approvals for software that uses artificial intelligence to read breast images and even predict future cancer risk from a routine mammogram. In June 2025 the FDA granted a De Novo authorization to Clairity Breast, the first AI platform authorized to predict a woman’s five-year risk of developing breast cancer using only a screening mammogram. This groundbreaking technology can spot suspicious findings and estimate future breast cancer risk, which can change follow-up and prevention strategies.
Other manufacturers have also received clearances or approvals for AI tools that assist radiologists by marking suspicious areas, incorporating prior exams, and improving detection in dense breasts. For example, iCAD’s ProFound Detection v4.0 earned FDA clearance in 2024. It reports improvements in detecting cancers in dense tissue and finding smaller, aggressive cancers. Major imaging vendors (Hologic, ScreenPoint/Transpara, and others) also offer FDA-cleared AI solutions that are already being integrated into many mammography workflows.
These FDA approvals reflect a rapid shift: there are now dozens of AI applications in breast imaging and a clear regulatory pathway for bringing them into clinical care and becoming a norm.
Why Might This Have a Major Impact on Our Community?
- Better detection in dense breasts and younger patients. Black women are more likely than some other groups to be diagnosed with breast cancer at younger ages and with aggressive forms. Dense breast tissue can make cancers harder to see on traditional 2D mammograms. Newer AI tools that detect subtle patterns in dense tissue can help find cancers earlier, which may help reduce disparities in outcomes.
- Personalized risk, not one-size-fits-all. Most traditional breast cancer risk tools were based on data from women of European ancestry and may miss risks for women of African descent. New AI tools can estimate 5-year risk from a mammogram, helping doctors tailor screenings and recommend extra tests for those at higher risk. The FDA’s recent approval marks a key step toward personalized care.
- More consistent reads and workload support. Radiologists’ experience can differ depending on the region and the facility. AI can act as a second reader or a triage tool, flagging cases that need urgent attention and helping reduce errors caused by human fatigue. Early programs using AI-assisted reading have shown lower workloads and faster triage times. In communities with limited access to breast imaging specialists, AI has the potential to improve equity—if it is implemented fairly.
AI Caveats
AI is powerful but not magic. There are three important concerns to keep in mind:
- Bias and representativeness. AI learns from the data it’s trained on. If training datasets don’t include enough Black women or images from diverse mammography systems, performance may drop for underrepresented groups. Developers and regulators are increasingly flagging the need for diverse datasets and post-market monitoring to ensure accuracy across populations.
- Access and implementation gaps. Having FDA clearance doesn’t automatically mean a hospital or clinic will adopt the tool. Facilities in historically under-resourced areas may lack the funding, infrastructure, or technical staff to install and maintain AI systems—so communities that could benefit most may be left behind unless payers and health systems prioritize equitable roll-out.
- Clinical integration and follow-up. An AI risk score is only useful if it leads to appropriate action: timely follow-up imaging, biopsy when indicated, and access to treatment. Social determinants—insurance, transportation, trust in healthcare—still shape outcomes. Tech that isn’t coupled with system-level investment in patient navigation and access won’t close survival gaps by itself.
FDA clearances for AI tools in breast imaging—especially the new approvals that predict short-term risk from a routine mammogram—are an exciting step forward. They create possibilities for earlier detection, more personalized screening, and reduced missed cancers. It also assists us in making informed decisions before feeling the pressure of a cancer diagnosis. But for the Black community to truly benefit, we must continue to become an advocate for health equity. Also, these technologies must be validated and trusted in our community; deployed equitably, reasonably priced (or covered by insurance) and paired with investments in access and follow-up.
Want to learn more about Breast Cancer and AI?
- Breast Cancer Research Foundation. “5 Takeaways from BCRF’s Webinar on AI and Breast Cancer Risk”
https://www.bcrf.org/blog/5-takeaways-from-bcrfs-webinar-on-ai-and-breast-cancer-risk/ - American Cancer Society. “New AI Tool Improves the Accuracy of a Breast Cancer Prognosis”
https://www.cancer.org/research/acs-research-highlights/breast-cancer-research-highlights/treatment-and-reducing-metastasis-studies-breast-cancer/new-ai-tool-improves-accuracy-breast-cancer-prognosis.html - BreastCancer.org.“Using AI (Artificial Intelligence) to Detect Breast Cancer”
https://www.breastcancer.org/screening-testing/artificial-intelligence - Nature Medicine.“AI-based selection of individuals for supplemental MRI in population-based breast cancer screening: the randomized ScreenTrustMRI trial”
https://www.nature.com/nature-index/article/10.1038/s41591-024-03093-5 - Breast Cancer Research Foundation.“AI Breast Cancer Detection and Diagnosis | Breast Cancer Screening”
https://www.bcrf.org/blog/ai-breast-cancer-detection-screening/ - AI and Breast Cancer poster. Elevate Black Health. https://www.elevateblackhealth.com/downloads/ai-and-breast-cancer/