Pain does not only live in the body. It speaks quietly but insistently to the mind, shaping mood, memory, and mental well-being. For the nearly 50 million U.S. adults coping with chronic pain, this dialogue often spirals into fatigue, anxiety, or depression. However, within the Black community, the conversation about pain and mental health takes on a sharper edge: bias and disbelief. Research shows Black patients are 40% less likely than White patients to receive medication for acute pain in emergency care. The ache may begin in the body, but when suffering is dismissed or disbelieved, the wound cuts deeper leaving scars on the psyche as well as the skin.
To understand the intersection of pain and mental health, think of the nervous system as an orchestra. Pain signals are the violins sometimes sharp, sometimes sustained, often impossible to ignore. The brain, conducting this complex performance, interprets those signals not in isolation but in concert with memory, emotion, and context.
Chronic pain, then, is not simply a matter of sore joints or stiff backs. It reshapes the brain’s wiring, dampening regions responsible for mood regulation and amplifying those tied to fear and anxiety. According to the American Psychological Association, individuals with chronic pain are three times more likely to develop depression or anxiety than those without.
In the Black community, however, that cycle is often left unbroken. For generations, mental health has not always been recognized as “real” or worthy of clinical care, leaving emotional pain to fester in silence. Layered on top of this is the long legacy of racial bias in medicine—particularly in pain management—where studies have shown Black patients are less likely to have their pain taken seriously or adequately treated. This history makes it even more urgent to acknowledge that pain does not respect boundaries of body or mind, and that both must be treated with equal care.
The Mental Toll of Medical Discrimination on Black Communities
Among Black individuals, the cycle of pain and mental strain is often intensified by disbelief. The record is clear. From 19th-century medical claims that falsely suggested Black people felt less pain to modern evidence of unequal access to pain treatment, bias has consistently shaped which voices are taken seriously in health care. A 2016 study published in Proceedings of the National Academy of Sciences revealed that half of medical students and residents surveyed still endorsed false beliefs about biological differences in pain perception between Black and white patients. These misconceptions directly shape care often resulting in Black patients being undertreated or dismissed.
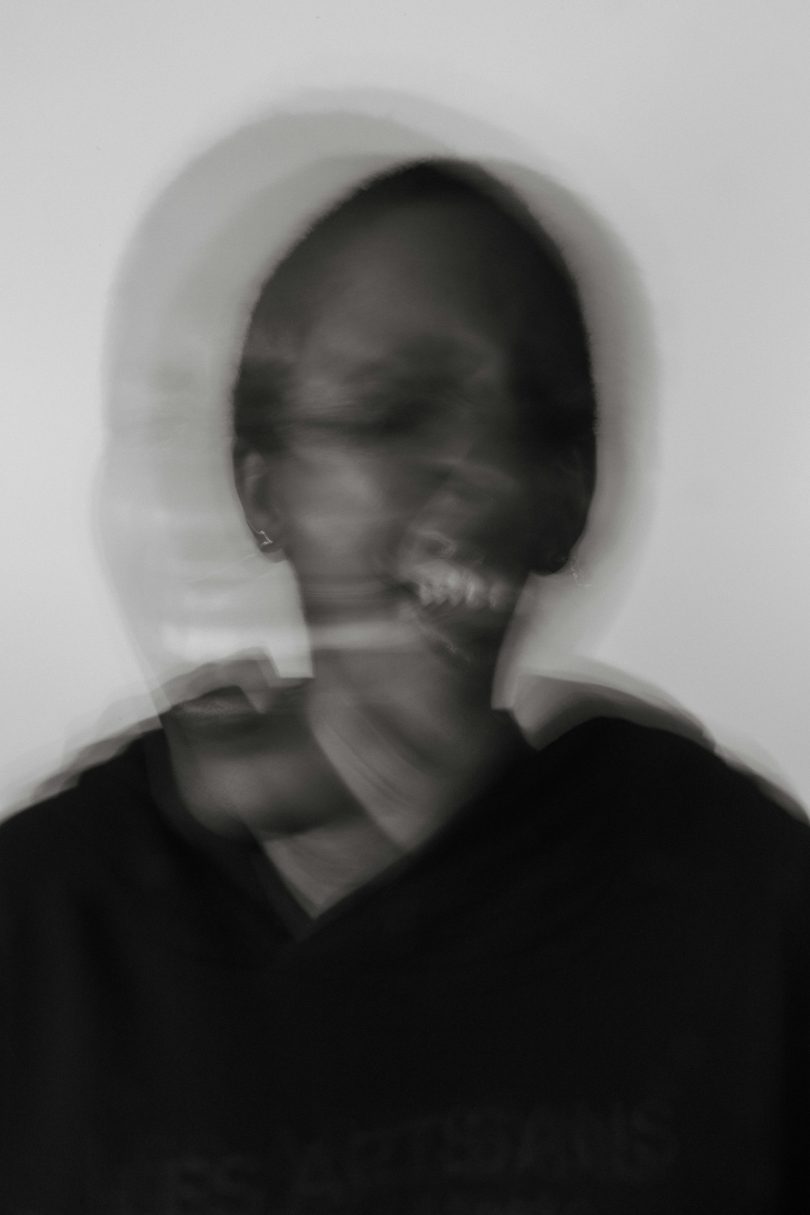
Imagine the psychological toll of walking into a clinic, seeking relief, and leaving not only in pain but also invalidated. Each dismissal is not merely a missed prescription; it is a message. The message says: your suffering is not worthy of our full attention. Over time, this repeated rejection becomes fertile ground for distrust, stress, and trauma.
That trauma has a name: weathering. Coined by public health researcher Dr. Arline Geronimus, the term describes how chronic exposure to social, economic, and health-related stressors accelerates aging and worsens health outcomes in our communities. Pain, untreated or undertreated, accelerates that weathering etching stress not only in the mind but also in the body’s very cells.
Steps Toward Lasting Solutions in Pain and Mental Health
If pain and mental health are threads of the same fabric, then solutions must be stitched with care, culture, and community at the forefront. Here are key steps forward:
- Culturally Competent Care: Healthcare providers must move beyond textbook definitions and acknowledge cultural context. Training in implicit bias is not enough; systems must hold practitioners accountable for equity in treatment. Black patients deserve care that affirms their experiences, validates their voices, and honors their pain
- Integrating Mental Health into Pain Management: Too often, treatment silos physical pain in one clinic and mental health in another. For Black patients disproportionately burdened by both, integrated care where psychologists, primary care physicians, and pain specialists collaborate is crucial. Holistic approaches like cognitive-behavioral therapy, mindfulness-based stress reduction, and group therapy can disrupt the cycle of pain amplifying anxiety
- Community-Based Interventions: Barbershops, churches, and community centers have long been hubs of healing and dialogue in Black culture. Leveraging these trusted spaces for pain and mental health education can reduce stigma and encourage early intervention. Programs that blend storytelling with science can empower individuals to see pain not as weakness but as a signal worthy of respect and response
- Patient Advocacy and Self-Advocacy: Knowledge is a powerful prescription. Encouraging patients to track their symptoms, bring advocates to appointments, and demand second opinions when dismissed helps shift power back into their hands. Organizations like the Black Women’s Health Imperative and the National Black Nurses Association offer resources tailored to navigating medical bias
- Research and Representation: Finally, more research on pain in Black populations is vital. Too often, clinical trials underrepresent Black participants, leaving a gap in data and solutions. Investment in inclusive research not only broadens scientific understanding but also signals to patients that their pain and their healing matters
The Dialogue Continues
Pain is universal, but the experience of pain is not. For individuals in our community, the body’s aches are too often intensified by society’s indifference, and the mind’s struggles are too often magnified by medicine’s mistrust. Bridging the chasm between physical pain and mental health requires more than prescriptions; it requires a reckoning.
Each ignored complaint, undertreated symptom, and invalidated voice adds weight to a burden already heavy with a complex history. Yet acknowledging this reality is the first step in rewriting the narrative. Pain does not have to be a prison, nor does it need to manifest into mental health struggles. With culturally attuned care, community support, and systemic accountability, pain can instead become a teacher, guiding us toward empathy, healing, and equity.
Further Reading:
Resilience in Rhythm: Music and Movement Heal. https://www.elevateblackhealth.com/resilience-in-rhythm-music-and-movement-heal/
Mental health care among blacks in America: Confronting racism and constructing solutions. https://pmc.ncbi.nlm.nih.gov/articles/PMC6407345/
How Music Helps People Heal: The Therapeutic Power of Music. https://www.harmonyandhealing.org/how-music-helps-people-heal/
Racism as a Source of Pain. https://pmc.ncbi.nlm.nih.gov/articles/PMC10212893/?
Pet Ownership and Mental Health. https://www.elevateblackhealth.com/pet-ownership-and-mental-health/